Do you assume today’s doctors, nurses and medical staff are satisfied with their work, dedicated to the medical field and confident that they are fulfilling their “calling”? Boy, are you ever wrong. I urge you to read my latest blog published by FierceHealthcare which has already generated an enormous number of comments, signaling that we’ve touched a nerve here. The real question is whether or not healthcare can see the challenge and respond to it quickly. As we conducted our interviews and research we found some common themes:
- This isn’t the type of job i thought i was going to have?
- This EMR is painful and not something i am comfortable doing?
- What happened to the compassion in caring?
- Where did this volume-driven “move them through” the system come from?
It didn’t matter if it was a doctor or a nurse. There is widespread pain in healthcare.
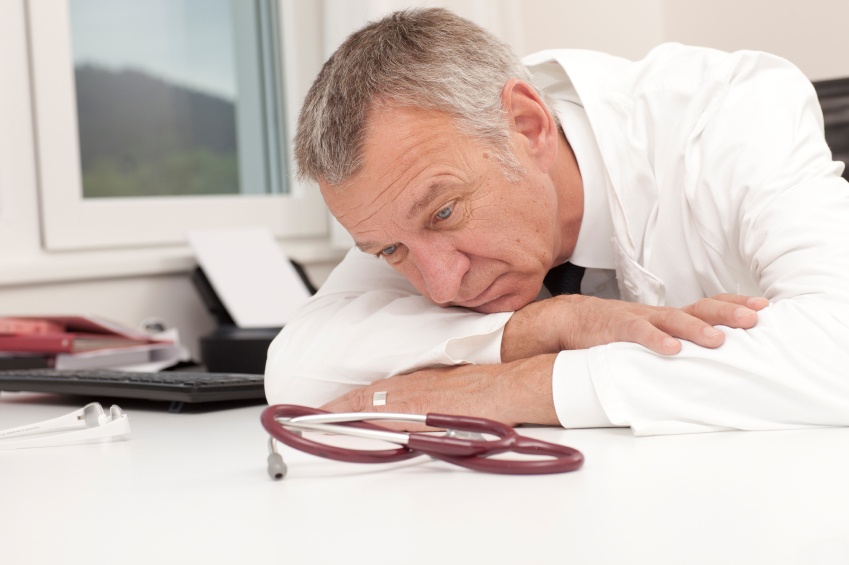
Faced with diminished compensation, consolidation of practices (ACOs) and constantly-shifting insurance structures, physicians are questioning their choice of careers. Nurses are working 12-hour, or even double, shifts. Every day, medical staff care for patients who are sick, ungrateful and often depressed. No wonder they’re burned out!
And the problem is not just here in America—it’s global. The same phenomenon is happening in Canada, South Africa, Finland, Taiwan, the UK, Holland, Spain and Latin America.
Not only is medical burnout a problem, it’s getting worse
- Burnout can occur in any occupation but happens most often in the “caring” professions: medicine, nursing, social work, counseling and teaching. Recent surveys reveal:
- U.S. physicians suffer more burnout than any other American workers
- 46 percent of all physicians report that they have burnout
- Burnout rates ranging from 30-65 percent occur across specialties, with the highest rates incurred by physicians at the front line of care, such as emergency medicine, critical care and primary care.
- Internists and family physicians were most likely to say they would not choose their own specialty again.
What begins as a calling often becomes an anchor dragging people down
Why should rates of burnout be higher among physicians? For one thing, they tend to work longer hours than other workers, on average about 10 more hours per week. Moreover, striking an appropriate work-life balance appears to be a bigger challenge for physicians, in part because they often tend to keep work and personal life more separated than other workers.
Burnout in the healthcare field is something we need to pay attention to, and fast
As a large portion of the U.S. population ages, the number of physicians caring for them will need to increase. When burnout causes physicians to reduce their practice or leave medicine altogether, patient access to healthcare is diminished. Also, burnt-out physicians are likely to be less productive, make more mistakes and generally deliver a lower quality of care than their more satisfied, fully engaged colleagues.
Instead, healthcare workers need to rediscover what attracted them to medicine in the first place, and healthcare organizations need to restructure their entire process so that medical personnel can experience earnest professional fulfillment. For more in-depth answers, watch this space for my follow-up blog, examining solutions to this alarming problem.
To read my blog in its entirety in FierceHealthcare, click here.